
What Causes Inflammation in the Body and How to Find Relief
Share
Inflammation is your body's built-in defense system. It’s a biological first responder that rushes to the scene of an injury or infection. But what happens when that protective response gets stuck in the "on" position? It can shift from a helpful, temporary fix to a key driver of chronic disease.
This lingering, low-level state of alarm, known as chronic inflammation, is what truly causes widespread problems, often fueled by modern lifestyle factors like a poor diet, relentless stress, and not enough sleep.
Understanding Inflammation: Acute Friend and Chronic Foe
Before we get into the triggers, it’s crucial to understand the two very different faces of inflammation. Think of your body's inflammatory response like an internal security team. One is a highly skilled, rapid-response unit that neutralizes a threat and goes home. The other is a patrol car that just keeps circling your neighborhood, sirens blaring, day and night.
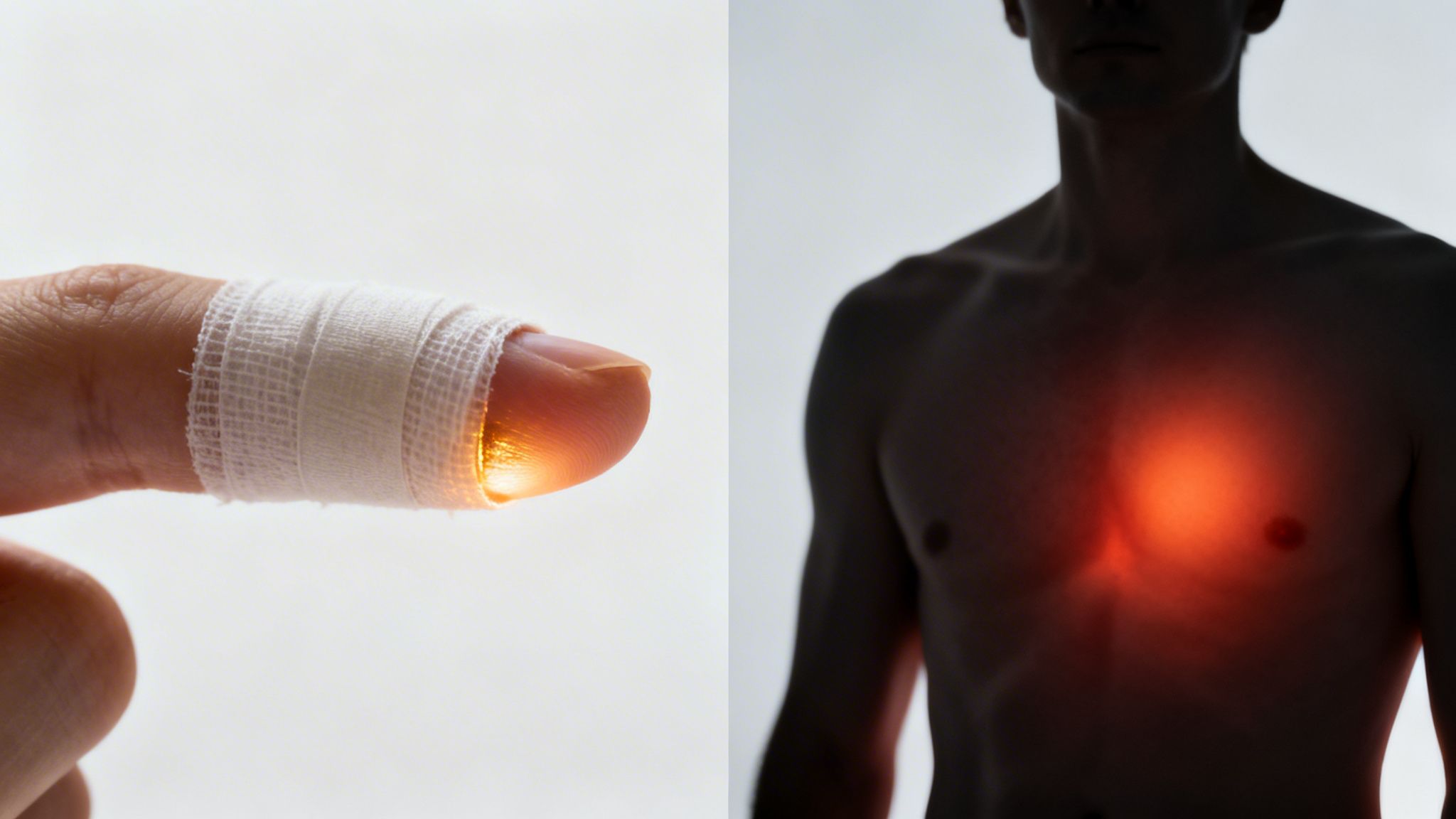
Acute Inflammation: The First Responder
When you get a paper cut, twist your ankle, or fight off a cold, acute inflammation is the first responder on the scene. This is your body's immediate, short-term, and life-saving defense strategy.
Imagine you've just sliced your finger. Your immune system instantly dispatches an army of white blood cells to the area. Blood vessels widen to give these cellular "paramedics" a clear path, which causes the familiar signs we all know: redness, swelling, and heat.
This response is targeted and efficient. It cleans the wound, fights off any invading bacteria, and kicks off the healing process. Once the job is done, the team packs up and stands down. Problem solved.
Chronic Inflammation: The Unrelenting Alarm
But what if that security team never gets the "all clear" signal? That's chronic inflammation. It’s a slow, smoldering, and low-grade state of alert that can simmer for months or even years, often without you realizing it.
Instead of a focused attack on a specific injury, this type of inflammation is systemic, meaning it affects your entire body. This unrelenting alarm keeps your immune system constantly activated, which can eventually wear down and damage healthy cells, tissues, and even your organs.
Chronic inflammation is a silent epidemic, with some estimates suggesting it affects nearly half of all adults. Modern research now links 60% of global deaths to diseases driven by chronic inflammation—a prolonged immune response that gradually degrades everything from our organs to our nervous system. You can read more about these findings from the Times of India.
Unlike the obvious signs of a sprained ankle, chronic inflammation often operates beneath the surface. It’s a major player in the development of today’s most common health issues, from heart disease and diabetes to autoimmune disorders and cognitive decline.
To get a clearer picture, let's break down the key differences side-by-side.
Acute vs. Chronic Inflammation At a Glance
This table offers a quick comparison to help you distinguish between the helpful hero and the hidden villain.
| Characteristic | Acute Inflammation (The Helper) | Chronic Inflammation (The Destroyer) |
|---|---|---|
| Onset | Immediate and rapid (minutes to hours) | Slow and insidious (days to years) |
| Duration | Short-term (a few days) | Long-term (months to a lifetime) |
| Primary Cells | Mainly neutrophils (first-responder immune cells) | Macrophages, lymphocytes, plasma cells (more advanced immune cells) |
| Visible Signs | Obvious: redness, heat, swelling, pain | Often subtle or invisible; symptoms are systemic (fatigue, pain) |
| Outcome | Healing, repair, and restoration of normal function | Tissue damage, scarring, and loss of function |
| Systemic Impact | Usually localized to the site of injury or infection | Affects the entire body, contributing to chronic diseases |
Understanding this fundamental distinction is the first step. Recognizing that one is a necessary, life-saving process while the other is a destructive, long-term state helps clarify why managing those lifestyle triggers is so critical for your long-term health.
The Science Behind Your Body's Inflammatory Response
To really get what's happening when inflammation flares up, we have to look at the incredible communication network running inside your body. When your system detects a threat—whether it’s bacteria from a cut or an invading virus—it doesn’t just panic. It launches a highly coordinated mission, directed by tiny but powerful messenger molecules.
This internal switchboard is the key to understanding both helpful, short-term inflammation and the damaging, chronic kind.
Cytokines: The Immune System's Messengers
Picture your immune cells as a SWAT team on standby. For them to work effectively, they need clear, instant orders. That's where cytokines come in. These small proteins are the immune system's primary signaling molecules, telling cells where to go, what to do, and when to stand down.
When a threat is found, certain immune cells release pro-inflammatory cytokines, which act like emergency flares shot into the sky. These signals rally other immune cells to the scene, crank up blood flow to the area (hello, redness and heat), and kick off the process of neutralizing the invader. It’s a brilliant, efficient system designed to protect and repair.
In a healthy response, once the danger is gone, your body sends out anti-inflammatory cytokines. These are the "all-clear" signal, telling the immune team their job is done. But with chronic inflammation, those pro-inflammatory signals never shut off, keeping your body stuck in a constant state of high alert.
This relentless signaling is like a fire alarm that just won’t turn off. The continuous flood of pro-inflammatory cytokines keeps immune cells activated, and eventually, they start damaging healthy tissues because they're always armed and ready for a fight that never really ends.
Oxidative Stress: Cellular Rust
Another key player driving chronic inflammation is oxidative stress. The best way to think about it is as a form of "cellular rust." It happens when there's an imbalance between damaging molecules called free radicals and the protective compounds we know as antioxidants.
Free radicals are unstable molecules that are a natural byproduct of your metabolism, but their numbers can skyrocket from exposure to pollution, processed foods, and too much sun. In small amounts, your body’s antioxidant defenses can handle them just fine.
But when free radicals start to outnumber your antioxidants, they go on a rampage, stealing electrons from healthy cells and damaging DNA, proteins, and cell membranes. This damage is a major red flag for your immune system.
This creates a self-feeding cycle:
- Initial Damage: An overload of free radicals injures your cells.
- Immune Response: Your immune system detects this damage and dispatches pro-inflammatory cytokines to clean up the mess.
- More Free Radicals: Here's the kicker—the inflammatory process itself generates even more free radicals.
This creates a vicious loop where oxidative stress triggers inflammation, which in turn produces more oxidative stress. It’s a huge reason why chronic inflammation can become so stubborn and destructive over time. To break the cycle, loading up on a diet rich in antioxidants and healthy fats is crucial. For anyone looking to support this balance, understanding the benefits of omega-3 fatty acids is a great place to start.
When you understand the roles of cytokines and oxidative stress, it all starts to make sense. You can see exactly how our daily lifestyle choices translate into internal chaos, giving us a clear map of how we can either fuel or cool the inflammatory fire within.
The Modern Triggers of Chronic Inflammation
While acute inflammation is your body’s rapid response to a clear threat, like an injury, chronic inflammation is more like a slow, smoldering fire. It’s a reaction to a constant, low-level assault from our daily lives. Think of it less like a five-alarm blaze and more like a faulty electrical circuit that’s always humming, slowly wearing down the entire system.
The modern world has a unique knack for keeping this circuit overloaded. These triggers rarely act alone; they often create a domino effect, locking the body in an inflammatory state. Pinpointing these sources is the first real step toward taking back control of your health.
Let's break down the most common culprits behind this persistent internal alarm.
This simple visual shows how a threat—like a virus or toxin—kicks off a chain reaction, releasing messenger molecules (cytokines) that ultimately lead to widespread cellular stress.
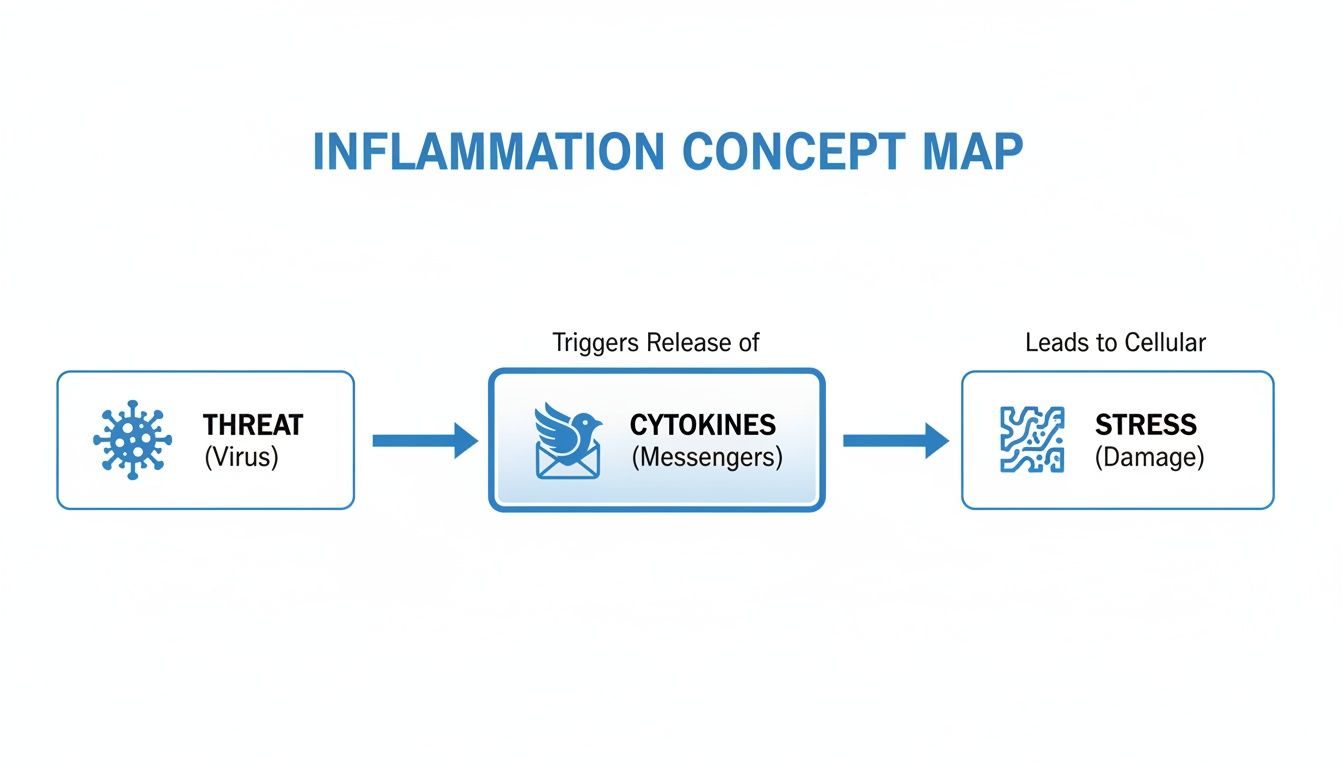
It’s a powerful sequence where one small trigger can unleash a cascade of biological responses that result in damaging, system-wide stress.
The Standard American Diet
The food you eat can be your most powerful anti-inflammatory tool or your primary source of inflammatory fuel. There's often no in-between. The Standard American Diet (SAD), packed with processed foods, refined sugars, and unhealthy fats, is a major driver of chronic inflammation.
Foods like sugary drinks, pastries, fried foods, and processed meats are treated by the body as foreign invaders. With every meal, they can trigger the release of pro-inflammatory cytokines, putting your immune system on high alert. This constant dietary stress disrupts gut health, spikes blood sugar, and creates the perfect storm for inflammation to thrive.
Excess Body Fat
We tend to think of body fat as just a passive energy reserve, but certain types are incredibly metabolically active—and not in a good way. Visceral fat, the kind that wraps around your organs deep within the abdomen, is especially dangerous.
This isn't just dormant tissue. Visceral fat acts almost like an endocrine organ, pumping out a steady stream of inflammatory cytokines directly into your bloodstream. It’s a relentless, 24/7 inflammation factory. The more visceral fat a person carries, the higher their baseline level of systemic inflammation is likely to be, which helps explain why obesity is a major risk factor for nearly every chronic disease.
Chronic Stress and Poor Sleep
Your mind and body are not separate. Mental and emotional stress directly translates into physical inflammation. When you're constantly stressed, your body floods itself with the hormone cortisol. In short bursts, cortisol is actually anti-inflammatory.
But when stress becomes chronic, your cells can become resistant to cortisol's signals. It's like your body's internal fire department stops responding to the emergency calls. This allows inflammation to run wild.
This vicious cycle gets even worse with poor sleep. Your body perceives a lack of restorative sleep as a major stressor, which spikes inflammatory markers. Even just one night of bad sleep can elevate these molecules, and chronic sleep deprivation keeps them dangerously high.
A Sedentary Lifestyle
Movement is one of the most potent anti-inflammatory medicines we have. When you exercise regularly, your muscles release compounds that have a powerful calming effect on inflammation throughout the entire body.
Living a sedentary lifestyle does the exact opposite. A lack of physical activity is strongly linked to higher levels of C-reactive protein (CRP), a key biomarker for inflammation in the blood. Inactivity also contributes to weight gain and poor metabolic health, adding more fuel to the inflammatory fire. You don’t have to run a marathon; consistent, moderate activities like brisk walking, yoga, or cycling all send the right signals.
An Imbalanced Gut Microbiome
Your gut is home to trillions of microorganisms that play a massive role in regulating your immune system. A healthy, diverse gut microbiome maintains a strong intestinal lining, which acts as a crucial gatekeeper between your digestive system and your bloodstream.
When this delicate ecosystem—the gut microbiome—is thrown off balance, a condition called dysbiosis occurs. The gut lining can become compromised or "leaky," allowing toxins and undigested food particles to escape into the bloodstream. This breach triggers a strong immune response and systemic inflammation.
Several modern factors can disrupt this balance:
- A diet low in fiber and high in processed foods
- Chronic stress
- Overuse of antibiotics
- Lack of physical activity
To dig deeper into the roots of inflammation, check out podcasts discussing the many things that cause inflammation in your body and how to address them. Understanding these interconnected triggers is the key to building a lifestyle that supports a calm, balanced internal state.
How to Recognize the Signs of Chronic Inflammation
Unlike the obvious, fiery swelling of a sprained ankle, chronic inflammation is much sneakier. It sends quiet, confusing signals that are all too easy to brush off as just being tired, stressed out, or getting older.
But learning to spot these subtle clues is the first real step toward connecting the dots and figuring out what causes inflammation in the body. These symptoms aren't dramatic—they're persistent and nagging. They’re the kind of issues that slowly chip away at your quality of life, leaving you feeling “off” without a clear reason why.
Listening to Your Body’s Whispers
The signs of chronic inflammation often show up systemically, meaning they can pop up anywhere in your body. It's not one big, glaring problem; it's a pattern of seemingly unrelated discomforts. Many people live with these feelings for years, never realizing they might all be connected to a single, underlying fire.
Paying attention is key. Here are some of the most common "invisible" symptoms to watch for:
-
Persistent Fatigue: This isn’t just feeling tired after a long week. It’s a deep, relentless exhaustion that a full night’s sleep can’t seem to touch. You wake up feeling like you never even went to bed.
-
Nagging Aches and Pains: Are you dealing with widespread body aches or joint stiffness, especially in the mornings, that have no clear cause? This is a huge red flag for systemic inflammation.
-
Brain Fog and Cognitive Issues: If you constantly feel like you're walking through a mental haze—struggling to focus, remember things, or think clearly—it could be a sign. Inflammation doesn’t just affect your body; it affects your brain, too.
-
Skin Problems: Your skin is often a mirror reflecting your internal health. Stubborn issues like eczema, psoriasis, mysterious rashes, or even adult acne can be outward signs of an internal inflammatory fire.
-
Digestive Troubles: Is gas, bloating, constipation, or diarrhea your constant companion? These are classic signs of an unhappy gut, which is a major hub for the body's inflammatory response.
The table below breaks down how these symptoms can appear across different body systems. You might notice a pattern that feels familiar.
Common Symptoms Linked to Chronic Inflammation
| Body System | Potential Symptoms |
|---|---|
| Neurological | Brain fog, memory problems, headaches, depression, anxiety |
| Musculoskeletal | Joint pain, muscle aches, stiffness (especially in the morning), weakness |
| Skin | Eczema, psoriasis, rashes, acne, premature aging |
| Digestive | Bloating, gas, constipation, diarrhea, abdominal pain, food sensitivities |
| General | Persistent fatigue, unexplained weight gain or loss, frequent infections, low-grade fever |
Recognizing these patterns is the first step. It shifts your focus from chasing individual symptoms to investigating the root cause.
Looking Deeper with Medical Tests
While listening to your body is crucial, a few blood tests can give you objective proof that inflammation is at play. If you suspect something is off, having an informed conversation with your doctor is the right next step. They can order specific lab work to get a clearer picture of what’s happening internally.
Two of the most common biomarkers for systemic inflammation are:
- C-Reactive Protein (CRP): Your liver produces this protein in response to inflammation. A special version of this test, the high-sensitivity CRP (hs-CRP), is particularly good at detecting the low-grade, chronic inflammation tied to long-term health risks.
- Erythrocyte Sedimentation Rate (ESR): This test sounds complicated, but the idea is simple. It measures how quickly your red blood cells settle in a test tube. Faster settling often means higher levels of inflammation in the body.
It’s important to remember that these tests are general indicators. They confirm that inflammation is present, but they don't tell you why. Think of them as smoke detectors—they alert you to a fire, but you still need to find the source.
When you combine these test results with your symptoms, you and your doctor can start building a real plan. Recognizing the signs is empowering. It’s the difference between feeling stuck and taking control, allowing you to finally start addressing the underlying issue.
Building Your Anti-Inflammatory Lifestyle

Knowing what’s fanning the flames is one thing, but actually doing something about it is where the real power lies. And the good news? Your daily habits are the most effective tools you have to cool down chronic inflammation.
You don't need to overhaul your entire life overnight. Instead, think about making small, consistent shifts across four key areas of your health. This isn’t about chasing perfection—it's about building a routine that sends calming signals to your immune system, day in and day out.
Fuel Your Body with Anti-Inflammatory Foods
Food can either be a primary trigger for inflammation or your most powerful medicine against it. The goal is to build a plate that’s heavy on whole, nutrient-dense foods that actively fight oxidative stress and help your immune system find its balance.
Start by loading up on foods rich in antioxidants—these are the compounds that protect your cells from damage.
- Colorful Fruits and Vegetables: Berries, leafy greens like spinach and kale, broccoli, and bell peppers are your best friends. The deeper and richer the color, the more protective compounds they usually contain.
- Healthy Fats: Don't fear fat! Sources of omega-3 fatty acids, like salmon, mackerel, walnuts, and chia seeds, are essential for producing your body's own anti-inflammatory molecules.
- Herbs and Spices: The power of your spice rack is seriously underrated. Turmeric (with its active compound curcumin), ginger, and garlic are all potent inflammation fighters.
At the same time, you'll want to dial back the pro-inflammatory stuff. We're talking about sugary drinks, refined carbs (white bread, pastries), fried foods, and processed meats. These foods can throw your blood sugar and gut health out of whack, keeping your body on high alert. For more on this, our guide on how to improve gut health naturally has some great, practical tips.
Embrace Consistent and Mindful Movement
Movement is a powerful modulator of your immune system. And you don't need to crush yourself with grueling workouts to see the benefits. In fact, for managing inflammation, consistency and moderation win every time.
Regular activity helps by circulating anti-inflammatory cytokines, managing weight (which reduces the inflammatory load from excess body fat), and improving insulin sensitivity. The secret is to find something you actually enjoy doing.
Think of moderate exercise as a reset button for your immune system. Each session helps flush out inflammatory markers and releases compounds that promote a state of calm, reinforcing your body's ability to self-regulate.
Try to build a balanced routine:
- Cardiovascular Exercise: Aim for at least 150 minutes a week of things like brisk walking, cycling, or swimming to boost heart health and lower key inflammatory markers.
- Strength Training: Building muscle is fantastic for your metabolic health, which is tightly linked to inflammation. Shoot for two or more sessions a week hitting the major muscle groups.
- Mindful Movement: Practices like yoga and tai chi are a double win, combining gentle physical movement with stress-soothing breathwork.
Prioritize Restorative Sleep and Stress Management
The connection between your mind and your inflammatory state is crystal clear. Chronic stress and bad sleep are a vicious cycle that keeps inflammation on a low boil.
When you're constantly stressed, your body pumps out cortisol. Over time, your cells can actually become resistant to its anti-inflammatory effects. Likewise, your body sees a lack of quality sleep as a major stressor, triggering a spike in pro-inflammatory signals.
Making 7-9 hours of quality sleep a non-negotiable priority is one of the best things you can do. Create a wind-down routine, ditch the screens before bed, and make your bedroom a cool, dark, quiet sanctuary.
To tackle daily stress, weave in simple mindfulness practices. This could be five minutes of deep breathing, a quick meditation, or just spending a little time in nature. For those looking to add other therapies, exploring the benefits of an infrared sauna for inflammation can be a great way to support symptom management. These small acts add up, significantly lowering your body's inflammatory burden over time.
When You Should Talk to a Doctor About Inflammation
Building an anti-inflammatory lifestyle is a powerful strategy, but it’s not meant to replace professional medical care. Knowing when to move beyond self-management and consult a healthcare provider is a critical part of taking charge of your health.
If your symptoms are severe, persistent, or starting to get in the way of your daily life, it's time to get a professional opinion. This allows you to partner with your doctor to dig deeper into what’s causing inflammation in your body, helping to either rule out or identify underlying conditions that require specific treatment.
Key Signs It’s Time for a Visit
Don't ignore symptoms that linger or seem to be getting worse. It’s a good idea to schedule an appointment if you experience any of the following:
- Persistent pain or stiffness that doesn’t get better with rest or gentle movement.
- Unexplained weight loss or gain when you haven’t made significant changes to your diet or activity level.
- Chronic fatigue that's so draining it disrupts your work, social life, or daily responsibilities.
- Symptoms of a possible autoimmune condition, like a butterfly-shaped rash across your face or recurring low-grade fevers.
Your doctor can run specific tests to get a clearer picture of what’s going on and may discuss more advanced treatments if needed. The global market for anti-inflammatory therapeutics is projected to reach around $164.44 billion, driven by the success of biologic drugs for complex conditions like rheumatoid arthritis and Crohn's disease. You can find out more about these therapeutic advancements on Precedence Research.
A professional can also check for nutrient deficiencies that might be contributing to the problem. That's why unlocking the health benefits of vitamin D3 supplementation is a conversation worth having with your provider.
Still Have Questions About Inflammation? Let's Clear Things Up.
Navigating the world of health can feel like learning a new language. As we've dug into what causes inflammation, a few key questions always seem to pop up. Here are some quick, straightforward answers to help everything click into place.
Is Inflammation the Same Thing as Infection?
Not quite, but they're closely related. It helps to think of it this way: an infection is the crime, and inflammation is the first responder team rushing to the scene.
An infection happens when an outside invader—like a virus or bacteria—gets into your body and starts multiplying. It’s the direct result of a harmful bug setting up shop where it doesn't belong.
Inflammation, on the other hand, is your body's reaction to that threat (or to an injury, like a sprained ankle). It’s the immune system dispatching white blood cells and other defensive compounds to neutralize the invaders and start the healing process. You can have inflammation without an infection, but you will always have inflammation with an infection.
Is All Inflammation Bad for You?
Absolutely not. In fact, acute inflammation is essential for survival.
It’s the powerful, short-term response that disinfects a cut, repairs a torn muscle, and helps you kick a cold. Without this protective mechanism, even a minor scrape could become a life-threatening problem.
The trouble starts when this emergency response gets stuck in the "on" position. Chronic, low-grade inflammation is the harmful kind. It keeps your body in a prolonged state of alert, which can eventually damage healthy tissues and pave the way for long-term health issues.
How Quickly Can I Reduce Inflammation?
This really depends on the root cause and how consistent you are with making changes. The good news is, you can start feeling the benefits of anti-inflammatory habits faster than you might think.
- Short-Term Changes: Within just a few days to a week of cleaning up your diet—think cutting out processed sugars and loading up on leafy greens and omega-3s—you might notice a real difference in your energy levels, digestion, and bloating.
- Long-Term Results: To see significant shifts in clinical markers like CRP or a real reduction in chronic pain, it generally takes several weeks to a few months of consistent effort. Lasting change is built on sustainable habits, not quick fixes.
The key is consistency. A single healthy meal won't erase years of inflammatory triggers, but every positive choice you make helps nudge your body back toward a state of balance. Small, daily actions build powerful momentum over time.
At Elemental Edge Health, we believe in giving you the tools to build a balanced, low-inflammation lifestyle. Our clean, research-backed supplements—from potent Omega-3s to antioxidant-rich greens blends—are designed to complement your daily efforts and help you feel your absolute best. Explore our full collection at https://www.elementaledgehealth.com.
